CBT for ADHD: How Cognitive Behavioural Therapy Helps Adults With ADHD
Learn how Cognitive Behavioural Therapy (CBT) helps adults with ADHD manage symptoms, build practical skills, and improve daily functioning.
CBT for ADHD
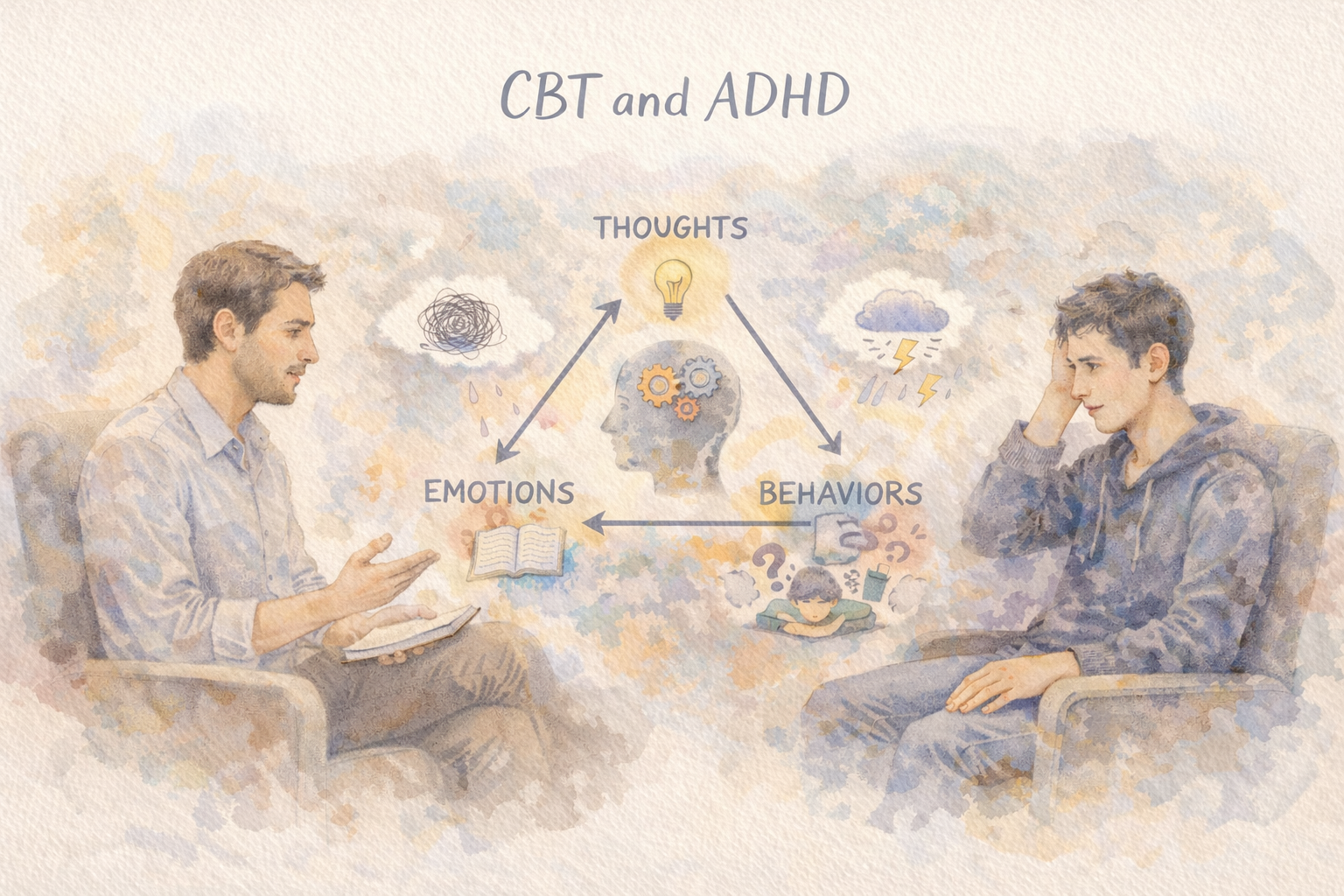
Cognitive Behavioural Therapy (CBT) has a strong evidence base as a psychological intervention for adults with ADHD. While ADHD is a neurodevelopmental condition, it significantly affects how people think, plan, organise, regulate behaviour, and manage everyday challenges. CBT targets these patterns directly.
Medication helps with core symptoms like inattention and impulsivity, but CBT teaches practical skills that improve day-to-day functioning and quality of life. It focuses on building strategies that work with the ADHD brain rather than against it.
This article explores how CBT works for ADHD, what happens in therapy sessions, how it differs from other approaches like DBT, what the research evidence shows, which techniques are most effective, and how adults in Australia can access CBT through psychology services and Medicare.
Why CBT Works for ADHD
CBT helps adults with ADHD by addressing unhelpful thought patterns and building practical behavioural strategies. Common ADHD-related challenges include:
Difficulty initiating or completing tasks
Negative self-talk and self-criticism
Feeling overwhelmed by complex or disorganised projects
Intense reactions to mistakes or setbacks
Perfectionism that triggers procrastination
All-or-nothing thinking
Difficulty setting priorities
Emotional reactions to forgotten commitments
CBT addresses these challenges through several mechanisms:
Cognitive restructuring helps people identify negative or unrealistic thoughts and develop more balanced perspectives.
Behavioural strategies provide step-by-step methods for improving organisation, time management, focus, and task completion.
Emotion regulation techniques help manage frustration, shame, overwhelm, and fear of failure.
The goal is building sustainable habits and self-monitoring strategies that persist long-term.
Research suggests CBT is often beneficial as an adjunct to medication, particularly for adults with residual functional impairment despite pharmacological treatment. It can also benefit adults who are unmedicated, cannot tolerate medication, or have not found an effective medication.
CBT vs DBT for ADHD: Understanding the Difference
These therapies serve different purposes and are often confused.
Cognitive Behavioural Therapy (CBT) focuses on thoughts and behaviours. It helps adults identify thinking patterns that create difficulty, then builds practical systems for organisation, scheduling, and task management. CBT is particularly useful for procrastination, disorganisation, task paralysis, and negative thought patterns that interfere with functioning.
Dialectical Behaviour Therapy (DBT) emphasises emotion regulation, distress tolerance, mindfulness, and interpersonal effectiveness. It addresses emotional impulsivity, rejection sensitivity, interpersonal conflicts, and intense mood fluctuations. DBT is often recommended when ADHD co-occurs with significant emotional dysregulation, self-harm risk, trauma, or borderline personality features.
DBT is not a first-line, guideline-recommended treatment specifically for core ADHD symptoms. It becomes relevant when emotional dysregulation or interpersonal challenges are primary concerns, but for executive function difficulties and organisation, CBT has stronger evidence support.
What Happens in CBT for ADHD
CBT for ADHD differs substantially from generic CBT for anxiety or depression. ADHD-specific CBT is highly structured, skills-focused, and action-oriented. Sessions address real-world problems and provide immediately applicable tools.
Assessment and Goal Setting
The psychologist conducts an assessment covering current ADHD-related challenges, work or academic functioning, daily routines, emotional triggers, existing coping strategies, and beliefs about productivity and capability. Together, the client and psychologist identify 3–5 specific, measurable goals such as reducing procrastination, establishing sustainable routines, or improving task completion.
Identifying Thought Patterns
Common cognitive patterns in ADHD include:
Catastrophising: believing imperfect performance will lead to disaster
Overgeneralising: extending single failures to broader self-judgments
Negative predictions: assuming futility before attempting tasks
Therapy helps recognise these patterns and understand how they drive avoidance and distress.
Cognitive Restructuring
Clients learn to distinguish facts from interpretations, question evidence for negative thoughts, generate balanced perspectives, and reframe mistakes as problems to solve rather than character flaws. This work reduces shame, fear of failure, and avoidance—major contributors to ADHD-related task paralysis.
Behavioural Strategies and Systems
This component forms the core of ADHD-specific CBT. Psychologists teach practical systems including the 5-minute start method, external reminders, daily planning templates, time-blocking with buffer periods, priority-setting frameworks, environmental modifications to reduce distractions, task breakdown strategies, and reward-based motivation approaches. Clients practice these between sessions through structured homework assignments.
Emotional Regulation
CBT helps identify triggers for emotional overwhelm—cluttered environments, missed deadlines, criticism, competing demands, or forgotten commitments. Clients develop techniques to pause, regulate, and re-engage rather than shutting down or avoiding.
Maintenance
Toward the end of treatment, clients create maintenance plans including warning signs of regression, backup routines, accountability structures, and personalised toolkits with step-by-step implementation guides for effective strategies. This supports continued progress after therapy concludes.
Research Evidence for CBT in Adult ADHD
Multiple systematic reviews and meta-analyses support structured CBT as an effective intervention for adults with ADHD, particularly for improving functional skills (planning, organisation, time management) and reducing ADHD-related distress and comorbid symptoms.
Research findings include:
Structured, ADHD-adapted CBT reduces procrastination, improves everyday executive functioning (organisation, time management), and decreases emotional distress. These improvements appear most clearly on self-report measures of real-world functioning.
For adults on medication with residual symptoms, adding CBT often provides additional benefit beyond medication alone. The combination addresses learned patterns, skills deficits, and non-functional systems that medication cannot change.
CBT frequently reduces anxiety and depression associated with ADHD, likely through improved functioning, increased self-efficacy, and reduced overwhelm from better organisational systems.
Some adults benefit from CBT without medication, particularly those who cannot tolerate medications, have not responded to pharmacological treatment, or prefer non-pharmacological approaches.
Important caveats: Effect sizes vary across studies and individuals. Benefits depend on receiving genuinely ADHD-adapted CBT (not generic CBT), completing homework assignments, and individual factors including comorbidities and life circumstances. Therapist training in ADHD-specific protocols matters significantly—generic CBT may be less effective. Improvements on self-reported executive functioning are more consistent than changes on objective neuropsychological measures. CBT teaches compensatory strategies and skills rather than changing underlying neurocognitive function.
Evidence-Based CBT Techniques for ADHD
These behavioural strategies are commonly used in ADHD treatment. They are most effective when practiced with psychologist guidance but can also be tried independently.
The 5-Minute Start
Task initiation presents greater difficulty than task completion for many adults with ADHD. Setting a timer for five minutes with a commitment only to begin often generates momentum that sustains continued work.
Task Breakdown
Rather than listing "clean room," break tasks into discrete steps: collect clothing, place dishes in sink, remove rubbish, clear desk surface. This creates frequent completion experiences and reduces overwhelm.
Simplified Thought Record
Traditional CBT thought records can be too complex for ADHD. A streamlined version includes: situation (what happened), automatic thought (immediate reaction), emotion intensity (0–100 scale), balanced alternative (another perspective), and immediate action step. This converts unhelpful thoughts into actionable responses.
Body Doubling
Working alongside another person, in-person or virtually, provides external structure that can improve focus and reduce avoidance. While this strategy is more common in ADHD coaching and community approaches than in formal CBT research, many adults find it beneficial.
Time-Blocking with Buffer Periods
Scheduling dedicated time blocks for tasks and adding 30–50% additional time reduces stress, lateness, and unrealistic scheduling.
Environmental Modifications
Rather than relying on willpower, modify the environment: remove phones from work areas, use website blocking software, make important items visible and accessible, designate specific areas for managing distraction impulses.
Reward-Based Motivation
Altered reward processing in ADHD means immediate reinforcement is particularly effective. Build in frequent, immediate rewards: brief breaks after focused work periods, small treats after completing sections, meaningful celebration after project completion.
Reset Routines
Taking 2–3 minutes between tasks for mental transition—brief tidying, stretching, breathing, reviewing next priorities—prevents chaotic task-switching common in ADHD.
Finding an ADHD-Specialist Psychologist
Psychologists specialising in CBT for ADHD provide structured tools and templates, assign homework between sessions, track progress systematically, troubleshoot ineffective strategies, teach both cognitive and behavioural skills, and adapt interventions to individual circumstances and needs.
This specialisation matters because generic CBT designed for anxiety or depression often does not translate effectively to ADHD. Adults with ADHD benefit from psychologists who understand that difficulties stem from executive function challenges, working memory limitations, and altered reward processing rather than motivation or willpower deficits.
Accessing CBT for ADHD in Australia
Medicare Rebates Through Mental Health Care Plans
GPs can provide Mental Health Care Plans enabling access to up to 10 rebated individual psychology sessions per calendar year through the Better Access initiative. Services are available with any registered psychologist (general or clinical) who provides CBT. Medicare rebates cover partial session costs—significant out-of-pocket fees typically remain.
Clinical vs General Psychologists
Both can deliver CBT. Clinical psychologists typically offer larger Medicare rebates but often charge higher fees, potentially resulting in similar out-of-pocket costs.
ADHD-Specialist Psychologists
Some psychologists focus specifically on ADHD-adapted CBT and executive functioning coaching. These specialists often understand ADHD challenges more comprehensively than general CBT providers. Resources including Psychology Today, the Australian ADHD Professionals Association (AADDPA), and headspace (for younger adults) can assist in locating ADHD-focused practitioners.
Telehealth Services
Many ADHD-focused psychologists offer telehealth throughout Australia, addressing long waitlists and limited local options, particularly in regional areas.
ADHD Coaching
Some adults work with ADHD coaches teaching behavioural strategies similar to CBT approaches. While potentially helpful, ADHD coaching is not Medicare-rebatable and typically costs more than subsidised psychology services.
Important Considerations
CBT is a treatment approach, not a diagnostic tool. It works best when ADHD has been properly assessed and comorbid conditions identified.
Comorbidities significantly influence outcomes. Anxiety, depression, substance use, sleep disorders, trauma, and autism affect which strategies work and what should be addressed first in treatment.
Individual responses vary. Some adults experience substantial, sustained improvement. Others require ongoing support or periodic booster sessions to maintain gains. This reflects both the chronic nature of ADHD and individual differences in treatment response.
Therapist expertise matters significantly. Look for specific training in ADHD-adapted CBT protocols, not just general CBT experience. Relevant questions include: "Do you use ADHD-specific CBT protocols?" "How many adults with ADHD have you treated?" "What does homework look like in your treatment approach?"
Conclusion
CBT for ADHD combines cognitive restructuring with practical skill-building to improve daily functioning. While it does not cure ADHD, it teaches strategies for working more effectively with ADHD.
Medication addresses core symptoms. CBT changes how people navigate daily challenges. For many adults, combining both approaches creates meaningful improvement in productivity, relationships, emotional wellbeing, and quality of life.
Adults in Australia can access CBT through GP referral for a Mental Health Care Plan. With appropriate support and evidence-based interventions, ADHD-related difficulties can become more manageable through learnable skills, sustainable systems, and effective strategies.
Kantoko: Doing ADHD Better
Research consistently shows that combining medication with CBT often provides the most comprehensive support for adults with ADHD.
At Kantoko, our clinicians specialise in ADHD assessment, diagnosis and medication management. Offering:
Comprehensive ADHD assessments for adults seeking diagnosis
Evidence-based medication management and titration
Ongoing monitoring and follow-up consultations
Telehealth appointments for convenient access nationwide
Ready to take the first step? Get started with us today.
This article is for informational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider for diagnosis and treatment options.

